 The NCRI is a not-for-profit organization founded in 2014 and became a 501(c)(3) tax-exempt organization on May 11, 2015 (EIN: 47-1740139). It was founded to examine commonalities among neurological diseases which cause considerable disability and burden to patients which include neurocognitive disorders, neuroinfections (poliomyelitis, tetanus, meningitis, encephalitis, etc.), tumor and developmental disorders, nutritional deficiencies (such as iodine deficiency, diabetes mellitus, etc.) and traumatic brain injuries (accidents, poisoning, falls, fires, unintentional and intentional injuries).
The NCRI is a not-for-profit organization founded in 2014 and became a 501(c)(3) tax-exempt organization on May 11, 2015 (EIN: 47-1740139). It was founded to examine commonalities among neurological diseases which cause considerable disability and burden to patients which include neurocognitive disorders, neuroinfections (poliomyelitis, tetanus, meningitis, encephalitis, etc.), tumor and developmental disorders, nutritional deficiencies (such as iodine deficiency, diabetes mellitus, etc.) and traumatic brain injuries (accidents, poisoning, falls, fires, unintentional and intentional injuries).
Since we were incorporated in 2014, we have been very clear about the purpose of the NCRI:
- We seek to conduct neuroscience research that paves the way for groundbreaking insights and treatments to the field. This is our primary reason for existing as well as the primary source motivation for us to accelerate progress that improves outcome and quality of life in patients. We obtain a significant proportion of our funding from independent sources, mostly individual donations, rather than from grants or corporations. This gives us the freedom to pursue research avenues without concern that those ideas be modified by others in the field who have their own research agenda and ideas, enabling us to explore the widest variety of clinical options.
- We learn much from our research efforts including:
- Educating our patients and contributors about how we develop new clinical solutions.
- Knowing what others are doing and finding in neurocognitive research and technology sectors, and in the medical community.
- Understanding what you can do to protect your own neurological health.
The NCRI goals include, but are not limited to: 1) discovering (through science) the sources of the neuropsychological problems which are known to exist in high numbers in society but are under-researched; 2) developing research paradigms to meet the urgent needs of those afflicted, and 3) disseminating new findings for promoting education and prevention of symptoms and 4) helping to empower patients through neurological evaluation and treatment advice.
Background
According to the World Health Organization, about 15% (about 1 out of every 7) of people in the world’s population have some type of neurological disorder and cause over 12% of total deaths globally—an extraordinary challenge to public health considering the advances in medicine made over the past century. The National Institute of Neurological Disorders and Stroke* lists over 600 neurological disorders affecting an estimated 50 million Americans each year and the list is growing. However, the single most salient reason that neurology lags behind other aspects of medicine is due to the limitations of having inadequate methods to actually study the brain—a situation that persisted for decades.
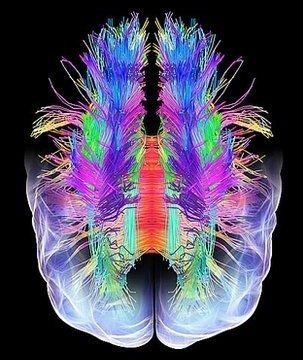
The NCRI conducts basic, applied and translational research using the newest and most innovative electrical neuroimaging techniques for defining relationships between patient symptoms and brain systems.
Advancements in neuroimaging since the 1990s permitted non-invasive study of the brain and today we are able to peer inside and look at the brain’s inner workings in real time to understand what events are happening, or not happening, during health or illness. Prior to this, doctors and scientists had to rely on a patient’s self-report, or wait until the patient died then perform an autopsy his or her brain. However, autopsies do not typically show the salient brain alterations taking place from the severe disruption in function and information flow as a result of the illness (cell death, cell weakness, etc.). Neuroimaging techniques which capture brain activity in real time have exponentially increased people’s interest in the brain and differential aspects of neurocognitive problems. This new ability–to model brain dynamics using new advancements in electrical neuroimaging (tomographic EEG)–has so revolutionized our understanding of the brain that we can now focus on specific brain states in disease processes which have been neglected or overlooked over the years.
While neurological diseases such as migraine syndrome, Alzheimer’s Disease, Lyme Disease, Parkinson’s Disease, multiple sclerosis, and epilepsy are more well-known, others are no less debilitating. For example, myalgic encephalomyelitis (a.k.a. chronic fatigue syndrome) is said to be a disease of unknown etiology, though findings demonstrate neuroinflammation, which is encephalitis.** ME affects an estimated 2.5 million people in the United States, costing up to $24 billion to society. Patients often report that symptoms of ME–unrelenting exhaustion and energy depletion as well as cognitive impairment–are the most debilitating aspects of the disease. Yet, less attention in the literature has been paid to underlying brain responses in cognitive impairment as reductions in cognitive performance are considered to be a sign of fatigue.
Our Story
Dr. Marcie Zinn was diagnosed in 2009 with herpes encephalitis (which further became myalgic encephalomyelitis). Herpes encephalitis is uniformly fatal within a few days if not caught immediately due to the intense inflammatory response associated with it, so about 7 out of 10 people die of herpes encephalitis. Read More >>
What We Do
The NCRI conducts basic, applied and translational research using the newest and most innovative electrical neuroimaging techniques for defining relationships between patient symptoms and brain systems. Functional relationships between different brain areas and their interactions give rise to cognitive processes. The systems approach to brain study allows researchers to gain insights into robustness or vulnerability characteristics of brain networks. It predicts that different network configurations present different patterns of vulnerability. Using a system approach, we can quantify physiological adaptations to chronic disease states to discover brain mechanisms for facilitating disease-modifying treatments, monitoring treatment progress, and obtaining meaningful and sustained health outcomes.
Further, the NCRI seeks to develop objective methods for classification with clinically relevant diagnostic indicators. In diseases such as ME/CFS, there is a need for establishing scientifically based diagnostic criteria which help identify and differentiate among similar clinical entities. Therefore, the NCRI fosters research to establish neural mechanisms specifically involved in various neurocognitive disorders and distinguished from other coexisting conditions.
The NCRI conducts preclinical research to practice prevention whenever possible since a number of cognitive deficits may be halted or even reversed if caught early on. We seek to develop and validate models predicting how the brain may react to multiple repeated insults in everyday life, to better understand how these insults affect cognition, helping people know when to seek treatment.
Finally, the NCRI promotes greater awareness in both medical community and general public as to the latest electrical neuroimaging methods, findings, and treatments of neurocognitive diseases. In this manner, we seek better access to health care resources, positive influence on public policy, and breaking barriers which challenge current assumptions in the field.
* The National Institute for Neurological Disorders and Stroke (NINDS) neglected to mention Chronic Fatigue Syndrome, Myalgic Encephalomyelitis, Myalgic Encephalomyelitis Syndrome, Chronic Fatigue and Immune Deficiency Syndrome, Systemic Exertion Intolerance Disease, etc. in its list of neurological disorders.
**The definition of encephalitis is inflammation of the brain. If this inflammation goes beyond a certain point, the person will die from the encephalitis (inflammation) alone.
About the Founders
